Symposium Recap From a Metastatic Breast Cancer Patient’s Perspective
Recently, I attended the Breast Cancer Symposium, a professional development conference for medical professionals who treat cancer patients; medical oncologists, surgeons, etc. This was the first year that patient advocates were invited to attend. Having patient representatives participate in these types of conferences can change the entire tone of the event since our priorities can differ from those of our doctors and it’s important to make them aware of that. There are many metastatic breast cancer patients who aren’t well enough to attend these types of events and advocate for themselves so I felt truly honoured to be included as a representative for MBC patients and I did my best to speak out on their behalf.
Many of the sessions involved discussions around de-escalation of treatment to minimize side effects while not increasing the risk of recurrence. It is the risk of recurrence that worries most breast cancer patients. Even a 3% to 4% increase can be significant if you are one of the patients within the 3% to 4% that experience recurrence. Research is advancing to identify the patients at greater risk of recurrence so that these patients can be offered the more aggressive treatment options.
As a metastatic breast cancer patient, my biggest concern is how my medical team will involve me in deciding which treatment is right for me. Will they outline a treatment plan, ensure that I understand it and get my approval? Or will they present me with treatment options, discuss the advantages / disadvantages of each option, try to understand my values and priorities and ask for my input in deciding which option is right for me? I would prefer the latter approach of shared decision-making. No one else can know what is most important for me so I want to be involved in my health care decisions.
Several physicians and patients attended the shared decision-making session hosted by Rethink Breast Cancer at the Symposium. Shared decision-making recognizes that both medical professionals and patients have a role in making treatment decisions. For example, a physician may inform a patient of clinical trial opportunities that are offered at their medical facility since they are easily accessible to the patient; however, the patient may be willing to travel to access clinical trials. If the doctor is unaware that the patient is willing to travel, their discussions may be limited to local clinical trial opportunities. If the doctor is aware that the patient is willing to travel (and how far they are willing to travel), additional clinical trial opportunities could be available for that patient.
For shared decision-making to happen
- Doctors need to understand their patient’s values, go beyond informed consent and make the patient part of the treatment team.
- Patients need to become actively involved in their treatment plan by asking questions to learn about alternate treatment options and voicing their opinion on what’s important to them.
The shared decision-making session included a very valuable discussion on the importance of this approach when treating cancer patients. Patient well-being improves when the medical team and patients work together to choose a treatment plan. At the end of the session, one of the physicians commented that this was the most valuable session of the entire Symposium. This is an encouraging sign that more physicians will begin to embrace shared decision-making.
Thanks to the chairs and organizers for accepting our presence at the Symposium. My biggest take-away is that while medical professional know a lot about medicine, it’s impossible to know everything. Doctors do not have a crystal ball and every patient is different. To ensure that your treatment plan is the right one for you, ensure that you become actively involved when there are decisions to be made.
For future sessions, I hope to see:
- More physicians participate in the “patient” session,
- More patient involvement in the “physician” sessions, perhaps as co-chairs,
- More medical professionals in attendance (nurse navigators, palliative care, etc.), and
- More patient-physician networking opportunities.
I look forward to being involved in further conversations with medical professionals and researchers to improve care for breast cancer patients.
To read more about the Canadian Breast Cancer Symposium, click here.

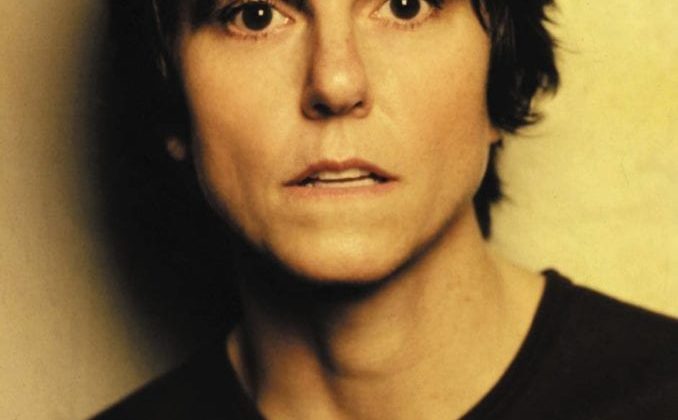
Nathalie Baudais was diagnosed with triple negative breast cancer in 2008, at the age of 29, and with metastatic breast cancer (MBC) in 2011. Her treatments have included multiple surgeries, chemotherapy regimens and radiation therapies. She has the BRCA1 genetic mutation. Nathalie is married and has one child. She works full-time and is involved with a variety of breast cancer charities: She is a board member for Saskatchewan Breast Cancer Connect; peer facilitator for Breast Cancer Support Saskatoon; organizing committee member for Breast Reconstruction Awareness (BRA) Day – Saskatoon. Nathalie is excited to be a part of the MBC advisory board and to help improve the lives of those living with MBC.